After suffering from depression for 10+ years, years of talk therapy and countless meds, I began my quest for an alternate treatment method. During a web search I stumbled upon Transcranial Magnetic Stimulation (TMS). It had positive reviews and was non-invasive, so I said what the heck. Let’s give it a try.
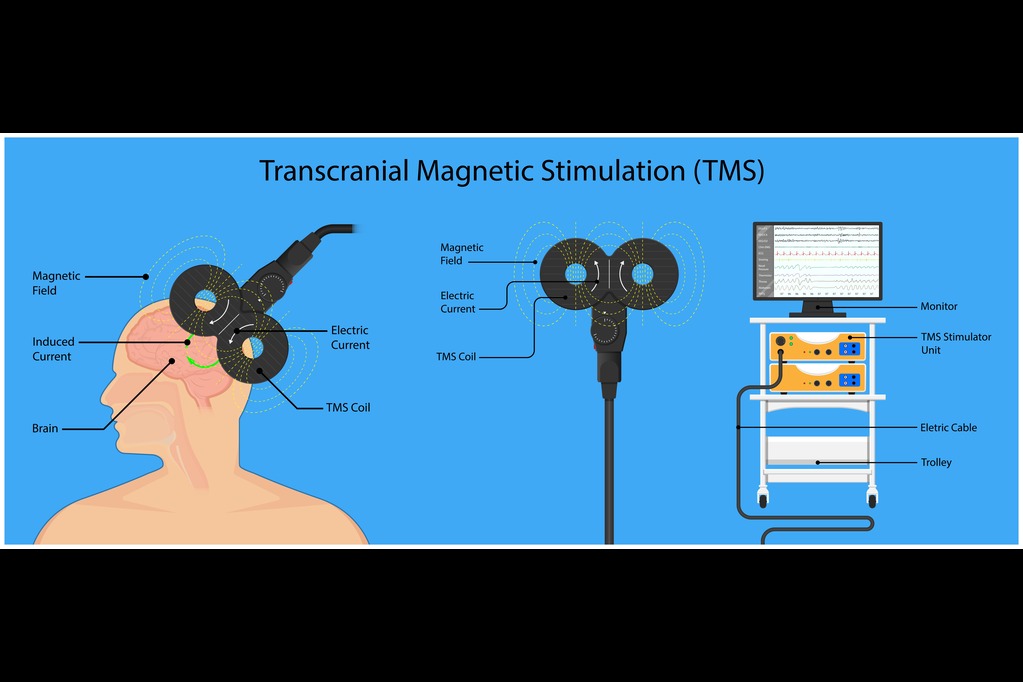
Transcranial Magnetic Stimulation (TMS) is a treatment method for depression when other modalities have failed. Magnetic pulses are emitted from a device (magnetic coil) placed on the patient’s scalp/head that focusses on a particular region of the brain. These pulses stimulate neural pathways in the brain that are associated with depression and mood. These neural pathways are thought to be under performing and the magnetic impulses stimulate these regions and cause new neural pathways to form in the brain.
We will discuss the following:
History Of TMS For Depression
TMS was approved by the Food and Drug Administration in 2008 as a treatment method for treatment resistant depression. It is an outpatient procedure that is provided in a clinicians’ office or a hospital. It has gained in popularity in its use for depression throughout the years, however, it still has a limited number of providers that offer the treatment.
The TMS Process
Finding a Facility
The first step is finding an office that offers TMS as a service and ensuring that insurance will cover it. A quick search in my state showed there are two facilities that offer TMS. As luck would have it, one of the treatment centers was located near our home. I scheduled a consult for 2 days out and off we go.
Bring Your Champion
My wife (Champion) and I went to the consult with the therapist to learn more about TMS and whether I would be a candidate for the treatments. It is important to have someone you trust at the consult. This could be your spouse, family member or friend. If memory ever becomes an issue they could be helpful. Also, it’s good to have another set of ears and someone to ask questions you may have forgotten.
The Consult
Testing
The therapist will perform a series of tests which will include the PHQ-9. It showed that I was in the severe depression range. Cognitive tests were also given to gauge the severity of my depression/set a baseline.
The interview
There will be an interview process where you will discuss the history of your depression including what you have tried as treatment methods so far. Such treatments include medications, talk therapy, etc.. You will also review health questionnaires with the therapist, outlining your current health state and medications.
The Ideal TMS Candidate
The ideal candidate will be a patient who has tried a series of medications for depression as well as psychotherapy and has not seen improvement. Conditions that may prevent the use of TMS would include certain types of implants, head trauma, etc. Your therapist will review these items with you during your consult.
The Crying
At some point during the consult I started to cry. These were tears that often come to light after/when I talk about myself and my condition.
There is no buildup, I just feel something in the pit of my stomach that moves into my head and bam. I head down the rabbit hole and lose control of my thoughts/emotions. The tears just flow. My most common feeling at the time is that I’m embarrassed that I am in a doctor’s office and need help. It’s a feeling of both sadness and anger. Basically, admitting that I am damaged and need help.
Treatment Options
The therapist will discuss alternative treatments other than medication. For me she noted three other than talk therapy and meds: TMS, Ketamine (Spravato) and ECT (Electroconvulsive Therapy). From an effectiveness standpoint, she said that ECT had the highest success rate.
Once she said this, I was all in. ‘Let’s do it.’ This seemed to catch the therapist off guard. Now the office offers ketamine and TMS as services. When I showed excitement, well not excitement, I’m depressed after all, let’s just call it a preference for ECT she stated that I’d have to be an inpatient in a hospital. Scratch that from my list. I was seeking an outpatient treatment.
Later, I would find the ECT statement regarding hospitalization to be inaccurate.
The Decision
I decided to try TMS in favor of the ketamine treatments (Sprovato) mainly because I feared panic attacks from Spravato. I have major control issues. I am a control freak. This is one of the reasons I am where I am. The doctor agreed that TMS was a good option for me. We set a day for me to come in to get my head mapped. This will help determine where the magnetic coil should be placed for my treatment.
Session 1 – Mapping
Your first appointment after the consult will be a mapping session performed by the therapist and/or technician. During this session, a magnetic coil will be placed on your head. The magnetic coil will be moved to different spots on your head to locate the part of your brain that causes your thumb to twitch. They do this by cycling the TMS machine from off to on, while moving the coil to find the sweet spot. You will feel a tapping sensation on your head and hear a series of loud clicks as the machine cycles.
After they find the sweet spot, they take measurements of your head to determine where they will place the TMS device for your treatments. They will target the dorsal lateral prefrontal cortex which for most people is where depression lives. The magnetic pulses will stimulate this part of the brain and other areas with the goal of stimulating the under functioning brain and creating new neural pathways (neuroplasticity – the brain’s ability to re-learn).
TMS Treatment Sessions
The patient will have 30 sessions over the course of 6 weeks, 5 days a week and 6 titration sessions. Sessions will last for +/- 18 minutes.
During a session, you will be provided ear plugs as the magnetic pulses emitted from the device are loud. Once the magnetic coil is placed in the correct position on your head, they will start your treatment.
The therapist/technician will leave the room after providing you with a ‘call’ button in case you experience any kind of distress. During the treatment, you will feel and hear a series of pulses (clicks) with short breaks between them.
Six Week Check-In
After 6 weeks of treatment, you will meet with the therapist and given the PHQ-9 again. Based on the results of the PHQ-9 and how you feel regarding the effectiveness of treatment, you will discuss the next steps. This may include discontinuing treatment or moving to theta bursts if you have not received the outcome you desire.
Theta burst stimulation (TBS) is the latest treatment method for those who traditional TMS has not been effective. This treatment session lasts for 3 minutes as opposed to 18+ with TMS and involves a more rapid magnetic stimulation at a higher frequency. The short of it is, TBS may work when TMS has failed.
The following video discuses the TMS process from mapping thru an actual session.
The Effectiveness of TMS
According to Harvard Heath, studies have shown that ‘50% to 60% of people with depression who have tried and failed medication(s) experience a clinically meaningful response’ with TMS. This may be a reduction of symptoms or becoming symptom free. As with many medical procedures, it may work, and it may not.
Although TMS treatments did not have a positive effect on me, they did get me out of the house and on a schedule. I met with the therapist at the 6 week mark and was given the PHQ-9 again. The results were the same as my initial PHQ-9 test. No improvement.
Pros of TMS Treatment
- The TMS treatment is non-invasive whereas ECT and Ketamine (Spravato) treatments are.
- Patient can drive themselves to and from sessions.
- No sedation is required.
- May be covered by Insurance. You’ll need to contact your insurance company.
- There is no downtime with TMS. You can return to daily activities after your TMS session has ended for the day.
- Depression symptoms may be reduced or eliminated.
Cons of TMS Treatment
- There is a time commitment. You’ll be expected to attend sessions 5 days a week for 6 weeks followed by 6 titration sessions.
- Availability. It may be hard to locate a provider in your region.
- Insurance will require prior authorization which can be tedious whereby you have to show that other treatment methods have been attempted and failed.
- Headaches
- Seizures
- It may not have an effect.
- Anxiety, both before and during treatment. As with anything new, especially within the medical world, anxiousness can play a role in your treatment.
- Extent of how long TMS will be effective is not known.
Summary
TMS is a treatment for major depression disorder when medications and talk therapy have not yielded the desired result. It involves sending magnetic pulses to the parts of the brain that deal with depression and mood. These pulses stimulate neural pathways in the brain. These neural pathways are thought to be under performing and the magnetic impulses stimulate these regions and cause new neural pathways to form in the brain. It is a noninvasive treatment taking place in a physician’s office or hospital that requires no downtime except for the therapy session. No anethesia is required. You can drive yourself to and from your appointment.
NOTE: My TMS Treatments occurred in 2022. There are now more TMS clinics in my state as it gains popularity.
DISCLAIMER: The information provided above is for informational purposes ONLY and should NOT be taken as medical advice.